

Trigger points (TrPs) or muscle “knots” are sore spots in soft tissue that cause deep aching. Myofascial pain syndrome (MPS) is a chronic pain disorder of too many trigger points. TrPs are usually described as micro-cramps, but the science is half-baked and their nature is controversial. Regardless, these sore spots are as common as pimples, often alarmingly fierce, and they seem to grow like weeds around injuries. They may be a major factor in back and neck pain, as a cause, a complication, or a bit of both.
There are many possible causes of unexplained aches and pains, but trigger points are an interesting piece of the puzzle for many people, and offer some potential for relief.
Trigger point therapy is mostly rubbing and pressing on trigger points, which can feel amazingly relieving. Dry needling is a popular (but dubious) method of stabbing trigger points into submission with acupuncture needles. TrP treatment is not rocket science 1 — it’s much too experimental to be so exact! But most people can learn to get some relief safely and cheaply.
This is a huge tutorial for both patients and professionals, regularly updated for more than a decade now. It’s a plainly written guide to all the science (such as it is), the myths and controversies, with reviews of every conceivable treatment option.

Does your body feel like a toxic waste dump?
It may be more true than you realized! Some data shows that a knot may be “polluted” with waste metabolites. If so, it’s no wonder they hurt … & hurt weird. It’s more like being poisoned than being injured. Back pain may be the best known symptom of the common muscle knot, but they can cause a startlingly wide array of other aches & pains.
Trigger point therapy isn’t “too good to be true” — it’s probably just ordinary good. It’s definitely not miraculous.2 It’s experimental and often fails. “Dry needling,” the trendiest type, bombed a good quality scientific test in 2020.3 Good therapy is hard to find (or even define), because many (if not most) practitioners are amateurish4 and some treatment methods are way out in left field and potentially harmful, to your wallet if nothing else. They are often barking up the wrong tree, treating so-called trigger points when there’s actually another problem.
There are no “trigger point whisperers.” Trigger points are not little switches that can be flicked off (“released”) by anyone who has sufficiently advanced technique — they are a mysterious, cantankerous, complex phenomenon. Any therapist who is highly confident about their ability to banish your sore spots should probably be fired.
Good trigger point therapy is hard to find but under-rated.5 It can be a safe self-treatment with the potential to help with many common pain problems that don’t respond well — or at all — to anything else.6 Done with care and humility, it’s worth dabbling in.
For beginners with average body pain — a typical case of unexplained nagging hip pain or low back pain or neck pain — the advice given here may well seem almost miraculously useful. I get a lot of email from readers thanking me for pointing out simple treatment options for such irritating problems. Some are gobsmacked by the discovery that their chronic pain could have been treated so easily all along.
For veterans who have already tried — and failed — to treat severe trigger points, this document is especially made for you. You should learn more before giving up. This could give you a fighting chance of at least taking the edge off your pain, and maybe that is a bit of a miracle.
This isn’t a guide to “fixing” trigger points; it’s a guide to giving you a fighting chance with tougher cases.
You’ve hit the jackpot if you’re serious about understanding muscle pain. This is the only tutorial of its kind: a book-length deep dive that isn’t just an advertisement for trigger point therapy. It’s an earnest and skeptical exploration of the biology and half-baked science of trigger points.
Attention physicians & therapists: The tutorial includes analysis of recent research that you won’t find in other texts, crafted for any skill level. Trigger points are more clinically important than most health pros realize, and body pain seems to be a growing problem.7 It’s a rewarding topic for doctors and therapists, a clear path to helping some people you probably couldn’t help before. Even if you already know about myofascial pain syndrome, you will get new ideas here.
I explore the nuances of all major ideas about trigger points, and review all the treatment options. This page has been improved and updated for 24 years — no joke, it has actually been here that long. Last update: Mar 4, 2024 (jump down to update log). Scientific rigour is my top priority; pseudoscientific ideas about trigger points are debunked here.
I am a former massage therapist,8 now a full-time science writer. I have also always been a “triggery” person and I suffer from chronic pain myself. ❐
Major sub-topics the tutorial will cover:
About footnotes. There are 479 footnotes in this document. Click to make them pop up without losing your place. There are two types: more interesting extra content, 1 and boring reference stuff. 2 Try one!
The “interesting” ones are mostly dorky digressions, clarification, context, whatever’s needed to fully inform a keen reader. And some are whimsical and silly, like this random selection from the PainSci comic archives…
“Boring” footnotes usually contain scientific citations from my giant bibliography of pain science. Many of actually do have interesting notes.
Example citation:
Acupuncture for Chronic Low Back Pain. N Engl J Med. 2010 Jul 29;(363):454–461. PubMed #20818865 PainSci #54942
About repeated citations: If I have already used a citation in footnote, I will mostly just link to that paper on subsequent references, especially if they are closely spaced. But if I am repeating it much further along and/or in a different context, I’ll give it another footnote and use op. cit. (“in the work already cited”).
A trigger point is a spot that is sensitive to pressure, mainly in muscle tissue, and often associated with aching and stiffness. 1213 Almost everyone gets these spots, like pimples, but some people get more of them, and more painful ones, and no one really knows what they are. They have had many names over the decades,14 but myofascial trigger point ( TrP ) is the trendiest and most widely accepted label in the last 20 years.
For much longer, TrPs are also informally known as muscle “knots.” Obviously it’s not a clove hitch or a bowline: there are no actual knots in there, but it can feel like that. And sometimes there’s some muscle hardness or lumpiness at the site, maybe embedded in a taut band of muscle — but these abnormal textures are hard to detect reliably, and even professionals routinely mistake normal anatomy for trigger points (or other abnormalities). Please don’t assume every spot/bump in your body is a trigger point. 😜
A few TrPs can get vicious for a while, causing far more discomfort than most people believe is possible. Its bark is much louder than its bite — these episodes will pass like a headache — but the bark can be painfully loud. It can also be a weird bark — trigger points can generate some odd and troubling sensations, and the source may not be obvious.
Although their true nature is uncertain, the usual story is that a trigger point is a small patch of tightly contracted muscle, a micro-cramp of a tiny patch of muscle tissue (as opposed to a whole-muscle spasm like a “charlie horse”15). And the story goes on: that small patch of muscle chokes off its own blood supply, which irritates it even more, a vicious cycle dubbed a “metabolic crisis.” This swampy metabolic situation is why I sometimes think of it as sick muscle syndrome.
But that could be wrong. A couple major competing ideas are that it’s a more purely sensory disturbance, or the pain of slightly irritated peripheral nerves, a type of peripheral neuropathy.
Trigger points aren’t just sensitive to pressure; they are also associated with aching and stiffness that spreads out around the TrP, even when you aren’t poking it. The TrP may be in the center of the aching, like the yolk of an egg, or the aching may spread surprisingly far away (via the mechanism of referred pain, another major sub-topic for later). It’s this aching that really puts the “syndrome” in myofascial pain syndrome…
A few minor trigger points here and there is a common annoyance, but a bunch of bad ones is myofascial pain syndrome ( MPS ), and it can be disabling. TrPs are to MPS as pimples are to a serious acne problem.
The more severe trigger points, the more extensive and severe the associated aching and stiffness. There are many other possible causes of unexplained pain, but trigger points are an interesting piece of the puzzle for many people, and knowing about them offers some potential for relief.
This is a fairly detailed summary, but we’re really still just getting started.

Although there are many causes of pain, confirming a trigger point diagnosis is simple enough for most people, most of the time. Check all that apply — if you have more than half of these, and no other apparent explanation for your pain, you probably have a trigger point or two.
Some symptoms that point away from trigger points: numbness, tingling, very sharp pain, joint pain, pain movement, abdominal pain, diffuse soreness or a widespread feeling of “fragility,” and malaise. But trigger points can and do co-exist with any other kind of painful problem.
We will go into even greater detail about symptoms below, because none of these items here are absolute, and the rules especially change for severe cases. For instance, no average trigger point will cause intense pain strongly linked to a specific movement… but severe ones can do that.
During a minor cyst removal from my chest many years ago, a potent stab of hot pain made me jump under the knife. “Very sorry,” the surgeon said. “I slipped and poked your pectoralis major with my scalpel, and only the superficial tissue is anaesthetized. Don’t worry, it won’t happen again.” And it didn’t. But I had learned a useful lesson: muscle tissue is sensitive stuff!17
Muscle pain matters. Aches and pains are an extremely common medical complaint,18 and trigger points seem to be a factor in many of them.1920 They are involved in headaches (including migraines),2122 neck pain and low back pain, and (much) more. What makes trigger points clinically important — and fascinating — is their triple threat. They can:
Muscle just hurts sometimes. Trigger points can cause pain directly. Trigger points are a “natural” part of muscle tissue.23 Just as almost everyone gets some pimples, sooner or later almost everyone gets muscle knots — and then you have some pain with no other explanation or issue.
It’s complicated. Trigger points complicate injuries and other painful problems. They show up like party crashers: whatever’s wrong, you can count on them to make it worse, and in many cases they actually begin to overshadow the original problem.
“It felt like a toothache.” Trigger points mimic other problems. Many trigger points feel like something else. It is easy for an unsuspecting health professional to mistake trigger point pain for practically anything but a trigger point. For instance, muscle pain is probably more common than repetitive strain injuries (RSIs), because many so-called RSIs may actually be muscle pain.24 A perfect example: shin splints.25
The daily clinical experience of thousands of massage therapists, physical therapists, and physicians strongly indicates that most of our common aches and pains — and many other puzzling physical complaints — are actually caused by trigger points, or small contraction knots, in the muscles of the body.
The trigger point therapy workbook, by Clair Davies, p. 2
Trigger point science is as disappointing as an empty Christmas stocking.26 Trigger points are under-explained and over-hyped. They aren’t a flaky diagnosis,27 but they’re not exactly on a solid scientific foundation either. Some critics have harshly criticized conventional wisdom about them — criticisms I’ll cover in detail later.
None of that is a deal-breaker, though: muscle pain is still an important topic, “trigger points” is a useful work-in-progress label for whatever is actually going on, and everyone agrees that something painful is happening. So all the more reason to have a rational tour guide to take you through a murky subject. What’s useful in the theory of trigger points? Who disagrees and why? What’s half-baked and obsolete? What are the major pitfalls? I critically analyze the topic from all sides.28
Sometimes half-baked ideas turn out okay if you just keep them in the oven. Trigger point science may be a bit of a hot mess, but it also isn’t over: the controversy about trigger points is a legitimate, interesting controversy. And meanwhile, as far as I know, I am actually the only author out there who is both promoting and criticizing trigger point therapy.
Family doctors aren’t really equipped for troubleshooting chronic pain.
Comic by Loren Fishman, HumoresqueCartoons.com
Trigger points are medically neglected because medicine has always had many much bigger fish to fry, and musculoskeletal medicine has only just recently started to get any real attention.29 Chronic pain with no obvious cause is a relatively unstudied epidemic and not many doctors know what to do with it and don’t even try.
If trigger points are a muscle tissue dysfunction or pathology — which is plausible but far from proven — that’s another reason they have fallen through the medical cracks: “Muscle is an orphan organ. No medical speciality claims it.”30 Muscle tissue is the largest organ in the body, complex and vulnerable to dysfunction, and full of biological puzzles.31 Although it is the “primary target of the wear and tear of daily activities,” nevertheless “it is the bones, joints, bursae and nerves on which physicians usually concentrate their attention.”32
Family doctors are particularly uninformed about the causes of musculoskeletal aches and pains33 — it simply isn’t on their radar. They are busy with a lot of other things, many of them quite dire. And the topic is just trickier than it seems to be, so it’s not really surprising that doctors aren’t exactly muscle pain treatment Jedi.
What about medical specialists? They may be the best option for serious cases. Doctors in pain clinics often know about trigger points, but they usually limit their methods to injection therapies — a bazooka to kill a mouse? — and anything less than a severe chronic pain problem won’t qualify you for admittance to a pain clinic in the first place. This option is only available to patients for whom trigger points are a truly horrid primary problem, or a major complication. Medical specialists may know quite a bit about muscle pain, but still can’t help the average patient for practical reasons.
An appallingly high percentage of doctors and other practitioners are still pretty much out of the loop regarding trigger points.
The trigger point therapy workbook, by Clair Davies, p. 2
Physical therapists and chiropractors are often preoccupied to a fault with joint function, biomechanics,34 and exercise therapy. These approaches have their place, but they are often emphasized at the expense of understanding muscle pain as a sensory disorder which can easily afflict people with apparently perfect bodies, posture and fitness. A lot of patient time gets wasted trying to “straighten” patients, when all along just a little pressure on a key muscle knot might have provided relief.
Massage therapists have a lot of hands-on experience of muscle tissue, but know surprisingly little about myofascial pain syndrome. Their training standards vary wildly. Even in my three years of training as an RMT (the longest such program in the world35), I learned only the basics — barely more than this introduction! Like physical therapists and chiropractors, massage therapists are often almost absurdly preoccupied with symmetry and structure. The right hands can give you a lot of relief, but it’s hard to find — or be — the right hands.
No professionals of any kind are commonly skilled in the treatment of trigger points. Muscle tissue simply has not gotten the clinical attention it deserves, and so misdiagnosis and wrong treatment is like death and taxes — inevitable! And that is why this tutorial exists: to help you save yourself, and to educate professionals.
Those clinicians who have become skilled at diagnosing and managing myofascial trigger points frequently see patients who were referred to them by other practitioners as a last resort. These patients commonly arrive with a long list of diagnostic procedures, none of which satisfactorily explained the cause of, or relieved, the patient’s pain.
Myofascial Pain and Dysfunction, by Janet Travell, David Simons, and Lois Simons, p. 36
The Big Red Books
Even atheists should be familiar with the Bible & every professional should have a copy of these books, despite their flaws.
In addition to many scientific papers, this tutorial is based on medical textbooks like the massive two-volume set, “the big red books” — Myofascial Pain and Dysfunction 36 — and “the blue book,” Muscle Pain 37 These are not easy reading.38
They don’t contain all the answers — indeed, they contain some nonsense — but anyone who claims to treat muscle pain should still have the big red books in their office. They are too historically important not to be familiar with. If you don’t see dog-eared copies of these books, ask about them — it’s a fair, polite clue about a therapist’s competence. Muscle Pain (the blue one) is just as important. I recommend it to any professional who works with muscle (or should). It’s more recent, and it covers a much wider range of soft tissue pain issues, putting trigger points in context.
Fibromyalgia ( FM ) is the disease of “hurting all over.” Fatigue, sleep disturbance, and “fibro fog” (mental confusion) are classic symptoms too. Fibromyalgia is a syndrome, not a disease, which means that it is unexplained by definition.39 It is just the label we give to undiagnosed chronic widespread pain. So “no one has FM until it is diagnosed.”40
MPS is just one of many possible explanations for the pain of fibromyalgia, and/or it might be a distinct meaningful diagnosis on its own. It would be nice if such a clear distinction were established someday. FM and MPS are both imperfect, imprecise labels for closely related sets of unexplained symptoms, which makes them harder to tell apart than mischievous twins who deliberately impersonate each other. They may be two sides of the same painful coin, or overlapping parts on a spectrum of sensory malfunction, or different stages of the same process. Some cases are effectively impossible to tell apart. There may be no real difference between FM and severe MPS.
Add to that the fact that both conditions are controversial to the point where some people deny they even exist, and it’s understandable that they get confused.
Note that the “tender points” of fibromyalgia are not the same thing as trigger points.41
Whatever the causes or labels, therapeutic approaches to MPS seem to help some FM patients as well,42 although pure FM cases seem to be mostly immune to massage.43 But this book is still useful for many FM patients, insofar as it overlaps with our main topic.
Fibromyalgic Tender Points
The “tender points” of fibromyalgia are not the same idea as myofascial trigger points.
I once suffered from a brutal “toothache” that was completely relieved by a massage therapist the day before an emergency appointment with the dentist: a particularly vivid experience, and one of the reasons I first got keen on this topic. Pain is a trickster; it is often not always what it seems to be. Trigger points are a common alternative explanation.
Got a bizarre pain that just flared up one day? Sure, it might be something scary or rare. But in many cases it’s probably just a trigger point — about as serious as banging your funny bone. But it can feel worrisome.
This is where trigger points really get interesting. In addition to minor aches and pains, muscle pain often causes unusual symptoms in strange locations. For instance, many people diagnosed with carpal tunnel syndrome are actually experiencing pain caused by an armpit muscle (subscapularis).44 Seriously. I’m not making that up.
This odd phenomenon of pain spreading from a trigger point to another location is called “referred pain.” Here are some other examples of interesting referred pain leading to misdiagnosis:45

Example of referred pain
The phenomenon of referred pain is one of the main reasons that trigger points can cause pain in unexpected places. This image shows a classic example. Many people have a sore spot in the upper gluteus maximus, but pain in this location often spreads either up into the low back and/or down into the rest of the gluteals & hamstrings. This pattern causes it to be widely misinterpreted as back pain and/or sciatica, when in fact it’s just a sore spot in the butt.
Sometimes trigger points cause such crazy symptoms that they are mistaken for medical emergencies. I treated a man for chest and arm pain — he had been in the hospital for several hours being checked out for signs of heart failure, but when he got to my office his symptoms were relieved by a few minutes of rubbing a pectoralis major muscle trigger point. “Heart attack cured!” The same trigger point sometimes raises fears of a tumor. Here’s a particularly excellent example sent to me by a physician who had this experience:
I narrowly escaped a breast biopsy because of trigger points in the pectoralis major. I’d had bad chest pain for a month. I was on the table, permit signed, draped. The doctor wasn’t sure: she said she wanted another mammogram. I left confused, relieved … but still hurting.
Then I lucked out: my regular internist was puzzled, but thought it might be “soft tissue.” That made me go to a physical therapist. The physical therapist pulled out the big red books on trigger points, and we read together. Treatment was a complete success. A month-old severe pain that I had been treating with ice packs in my bra and pain-killers — gone!
Janice Kregor, competitive swimmer, retired pediatrician and medical school instructor
Another client once spent three days in hospital for severe abdominal pain that doctors couldn’t diagnose — her pain was mostly relieved by massaging a trigger point in her psoas major muscle.51
But most symptoms caused by myofascial pain syndrome are simply the familiar aches and pains of humanity — millions of sore backs, shoulders and necks. Some of which can become quite serious.

Is this like you?
Muscle knot pain can be savage. Over the years I have met many people who were in so much pain from muscle dysfunction that they could hardly think straight. Is muscle pain “trivial”? Not if you have it!
The link between trigger points and mild-to-moderate body pain can be so straightforward that “therapy” is so easy it barely deserves to be called therapy. One of the nice things about working with trigger points is that, sometimes over the years, they have made me seem like a miracle worker… because they are such a clinical slam dunk for some cases of garden variety persistent pain.
For instance, Lois McConnell of Vancouver came to see me complaining that she’d had moderate, chronic back pain for several years. She’d received some common misdiagnoses, particularly sacroiliac joint dysfunction.52 But she had a prominent gluteus maximus trigger point53 that, when stimulated, felt exactly like her symptoms — a deep ache in the region of the low back and upper gluteals. Her pain was permanently relieved in three appointments. She was quite pleased, I can tell you!
Just wanted to give you a quick update … my back has been absolutely fine. Unbelievable … or perhaps not, considering what I’ve learned from you! A big thank you for all your help.
Lois McConnell, retired airline executive, suffered chronic low back and hip pain for a few years
Or consider Jan Campbell. Jan developed a hip pain sometime in early 2004 during a period of intense exercising. The pain quickly grew to the point of interfering with walking, and was medically diagnosed as a bursitis, piriformis strain, or arthritis. “Ain’t nobody got time for that.” I did not think any of these were likely, and treated a trigger point in her piriformis muscle once on June 12, 2004. Her symptom was 100% relieved for about eight months, before it slowly began to reassert itself (as trigger points often do, despite our best efforts — more about that to come).
One trigger point therapy treatment completely relieved a nasty stubborn hip pain that I'd had for five months!
Jan Campbell, retired French language teacher, Palm Springs, recovered easily from several months of hip pain
Every decent trigger point therapist has a pack of treatment successes like this. (Not that therapists are great judges of their own efficacy,54 but where there is this much smoke…) Although most such cases involve relatively minor symptoms, this is not to say that they were minor problems. In almost every such case, the pain was relatively mild but extremely frustrating and persistent for many years, then relieved easily by a handful of treatments — an incredible thing, when you think about it. So much unnecessary suffering!
But of course trigger points don’t always yield so easily…
Can a good enough massage therapist remove all trigger points in a session? Is there such a thing as a “trigger point whisperer”?
I got this question by email, and it exposes a common theme: the optimistic/desperate quest for the mystique of the magic super therapist who can fix anything in two or three sessions. Or even less.55 The idea is exasperating to all the honest, humble professionals who know better. And, if you know the basics about pain and muscle knots, it’s obviously foolish. The skill of a therapist is actually only one relatively minor factor among many that affect the success of massage therapy for trigger points — or any therapy, for any pain problem.
Trigger points are not little switches that can be flicked off (“released”) by anyone who has sufficiently advanced technique — they are a mysterious, cantankerous, complex phenomenon. Even the best therapists can be defeated by a no-win situation and factors beyond their control.56 And nearly any therapist can luck out and get great results with the occasional patient when all the planets are aligned: sometimes trigger points respond well to virtually any intervention.
For comparison, can a good enough dog trainer train any dog in a hour? Even Cesar “Dog Whisperer” Millan says he can’t if the dog is traumatized, sick, and/or injured, and requires hours of smart, gradual conditioning. It depends on the situation.
It depends, it depends, it depends. This is a major theme in this document, and it is why I am dedicated to teaching concepts and principles, not treatment recipes and formulae — and that’s why it’s an important thing to cover in the introduction.
How can you tell if trigger points are the cause of your problem?
Trigger points have many strange “features” and behaviours, and can easily be confused with many other common undiagnosed causes of pain in general57 and muscle pain in particular. There are several common kinds of muscle pain, or pains that can seem like it: arthritis, medication side effects, exercise soreness, muscle tears, and the profound body aching caused by an infection like COVID-19.58 The only hope of telling these things apart is a good working knowledge.
Thanks to their medical obscurity and the half-baked science, trigger points are often the last thing to be considered. There are some clues you can look for that will help you to feel more confident that, yes, this kind of muscle pain is the problem instead of something else, maybe something scarier.
Whether you knew it or not, you were probably already familiar with trigger points even if you’d never heard of them before laying eyes on this page. Almost everyone more or less knows what it feels like to have a muscle knot, so almost everyone has a head start in self-diagnosing trigger points. If you’ve ever been inexplicably stiff — and really, who hasn’t? If you’ve ever wrenched your neck around trying to stretch and squirm your way free of discomfort. If you’ve begged a boyfriend to dig into that nagging sore spot in your back. If you had experiences like those, then you already know something about what trigger points feel like: pain and stiffness that feels like it’s in your muscles, sensitive patches of soft tissue in locations where there’s no obvious reason for it.
But, Padawan learner, there may be many things you do not yet know about how trigger points behave and feel…
Purchase full access to this tutorial for USD $ 19 95 . Continue reading this page immediately after purchase. See a complete table of contents below. Most content on PainScience.com is free. ?
Almost everything on this website is free: about 80% of the site by wordcount, or 95% of the bigger pages. This page is only one of a few big ones that have a price tag. There are also hundreds of free articles, including several about trigger points. Book sales — over 73,900 since 2007 ? This is a tough number for anyone to audit, because my customer database is completely private and highly secure. But if a regulatory agency ever said “show us your math,” I certainly could! This count is automatically updated once every day or two, and rounded down to the nearest 100. Due to some oddities in technology over the years, it’s probably a bit of an underestimate. — keep the lights on and allow me to publish everything else (without ads).
A. I know it can make a poor impression, but I have to make a living and this is the best way I’ve found to keep the lights on here.
![]()
Paying in your own (non-USD) currency is always cheaper! My prices are set slightly lower than current exchange rates, but most cards charge extra for conversion.
Example: as a Canadian, if I pay $19.95 USD, my credit card converts it at a high rate and charges me $26.58 CAD. But if I select Canadian dollars here, I pay only $24.95 CAD.
Why so different? If you pay in United States dollars (USD), your credit card will convert the USD price to your card’s native currency, but the card companies often charge too much for conversion — it’s a way for them to make a little extra money, of course. So I offer my customers prices converted at slightly better than the current rate.
read on any device, no passwords
refund at any time, in a week or a year
call 778-968-0930 for purchase help
| company | PainScience.com |
|---|---|
| owner | Paul Ingraham |
| contact | 778-968-0930 |
| refunds | 100%, no time limit + Customers are welcome to ask for a refund months after purchase — I understand that it can take time to decide if information like this was worth the price for you. |
| more info | policies page ❐ |
| payments |
A. Payment unlocks access to 168 more chapters of what is basically a huge webpage. There is no paper book — I only sell book-length online tutorials. This format is great for instant delivery, and many other benefits “traditional” e-books can’t offer, especially hassle-free lending and updates. You get free lifetime access to the always-current “live” web version (and offline reading is easy too).
Read on any device. Lend it out. New editions free forever.
A. The design and technology of the book is ideal for reading on tablets and smart phones. You can also print the book on a home printer.
A. Yes! Feel free to lend your tutorial: I do not impose silly lending limits like with most other ebooks. No complicated policies or rules, just the honour system! You buy it, you can share it. You can also give it as a gift.
A. Literally safer than a bank machine. Payments are powered by Stripe, which has an A+ Better Business Bureau rating. Card info never touches my servers. It’s easy to verify my identity and the legitimacy of my business: just Google me [new tab/window].
A. Yes. All PainScience.com ebooks have a lifetime money-back guarantee.
A. To prevent fraud and help with order lookups. You aren’t “subscribing” to anything: I never send email to customers except to confirm purchases.
A. Not yet. Maybe someday.
See the “fine print page” for more about security, privacy, and refunds. No legalese, just plain English.
The e-boxed set is a bundle of all 10 book-length tutorials for sale on PainScience.com: 10 books about 10 different common injuries and pain problems. All ten topics are (all links open free intros in a new tab/window): muscle strain, muscle pain, back and neck pain, two kinds of runner’s knee (IT band syndrome and patellofemoral pain), shin splints, plantar fasciitis, and frozen shoulder. (Headache coming soon, fall of 2019.)
Most patients only need one book, because most patients have only one problem. But the set is ideal for professionals, and some keen patients do want all of them, for the education, and for lending to friends and family. And, of course, you do get a substantial discount for the bulk purchase. But no rush—complete the set later, minus the price of any books already bought. More information and purchase options.
“The clarity of your writing is very impressive, and you bring a great attitude to it.” ~ Brittney Taylor
“One trigger point therapy treatment completely relieved a nasty stubborn hip pain that I'd had for five months!” ~ Jan Campbell, retired French language teacher, Palm Springs, recovered easily from several months of hip pain
“Thanks to your website, I pretty much got rid of my back problems almost overnight. It’s also fun and thought provoking to read!” ~ Amsterdam Jeroen Strompf, MFA, Screenwriting, Chapman University
print, save & lend
read on most devices
new editions FREE forever
money-back guarantee
all myths & controversies
all diagnostic issues
all treatment options
Sign-up to get the salamander in your inbox, 1–3 posts / week depending on coffee intake, mostly short: interesting study results, rehab and treatment tips, rants, reviews, recommended reading, excerpts and updates from around the site, and more.
Or get premium posts
& support the salamander with PainSci Membership. See also “better” and “awesome” plans.
Join for $ 3/month or $ 30/year USD
You can also keep reading more without buying. Here are some other free samples from the book, and other closely related articles on PainScience.com:
![]()
Paying in your own (non-USD) currency is always cheaper! My prices are set slightly lower than current exchange rates, but most cards charge extra for conversion.
Example: as a Canadian, if I pay $19.95 USD, my credit card converts it at a high rate and charges me $26.58 CAD. But if I select Canadian dollars here, I pay only $24.95 CAD.
Why so different? If you pay in United States dollars (USD), your credit card will convert the USD price to your card’s native currency, but the card companies often charge too much for conversion — it’s a way for them to make a little extra money, of course. So I offer my customers prices converted at slightly better than the current rate.
read on any device, no passwords
refund at any time, in a week or a year
call 778-968-0930 for purchase help
A. Not really, but in a way: thirteen classic trigger points are explored in separate (free) articles, the “Perfect Spots” for massage (check out #1), which are associated with many common pain problems. But charts tend to put the focus on the wrong thing, and people need principles way more than they need diagrams. In any case, there are lots of good free/cheap charts out there. Please don’t buy this book and then ask for a refund because it doesn’t have charts: it’s like asking for a refund for your zoo admission because you didn’t see any cats, dogs, or squirrels!
A. Probably not, but maybe! Many specific pain problems are mentioned briefly, but the book doesn’t go into detail about any of them. You don’t really need the link to every common pain problem spelled out. Trigger points cause and complicate all injuries in fairly predictable ways — that’s why they are clinically intriguing!
There’s a lot of overlap with widepsread, non-specific chronic pain — like fibromyalgia — so I get into those topics quite a bit too.
A. Clair and Amber Davies’ popular book is written well. It’s illustrated nicely, and offers detailed muscle-by-muscle reference material — things this tutorial deliberately lacks.
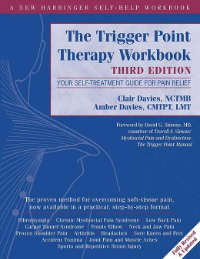
The Workbook promises too much & neglects relevant science.
(This is a very short version of my full review.)
I used to wonder why I even bothered to create this tutorial! Why not just recommend the Workbook ? Because this tutorial has grown to offer a lot that the Workbook doesn’t.
Delving into the nature of the beast — the science — is the strength of this tutorial. But the Workbook has fallen behind the times on that score. The current edition still promises too much and neglects important new knowledge. Trigger point therapy has been challenged by many scientific insights and new ways of understanding pain, but the Workbook doesn’t acknowledge any of that. This topic is too important for such neglect.
This tutorials offers a more realistic and balanced view of trigger point therapy, meets the challenge of difficult cases head on, and hard-nosed reviews of every possible treatment option. All for $20. Which is quite a bit less than even a single appointment with someone who claims to do trigger point therapy.
![]()
Paying in your own (non-USD) currency is always cheaper! My prices are set slightly lower than current exchange rates, but most cards charge extra for conversion.
Example: as a Canadian, if I pay $19.95 USD, my credit card converts it at a high rate and charges me $26.58 CAD. But if I select Canadian dollars here, I pay only $24.95 CAD.
Why so different? If you pay in United States dollars (USD), your credit card will convert the USD price to your card’s native currency, but the card companies often charge too much for conversion — it’s a way for them to make a little extra money, of course. So I offer my customers prices converted at slightly better than the current rate.
read on any device, no passwords
refund at any time, in a week or a year
call 778-968-0930 for purchase help
Decades of experience and study … reduced to a few bullet points. 😉
Every one of those points is the tip of an iceberg. The devil is in the details, and that’s why there’s a very large book about them behind the paywall. But this summary should help give you a better sense of whether or not you want to learn more from this source.
Where are Appendices A and B? They are included in the full, paid version of this document. This section is included as a free sample, like the introductory sections.
This is a list of resources relevant to chronic pain in general, but muscle pain in particular. I avoided publishing this section of the tutorial for many years, because I am generally not impressed by the resources available (to both patients and professionals), especially online resources. I remember a slightly testy conversation with someone from an American organization (that shall remain nameless):
| THEM | You say it’s hard for patients to find good trigger point therapy. You shouldn’t say that! We certify good trigger point therapists! |
| ME | You have about fifty practitioners in your directory, concentrated in a handful of major cities, with a certification no one has ever heard of, for a country of more than 300 million people spread over almost 10 million square kilometres. That’s one certified therapist for about every 60,000 people and 200,000 square miles. If “needle in a haystack” is the new “easy to find,” then sure, I’ll say that your certified therapists are easy to find. |
| THEM | Well, you still shouldn’t say that it’s hard to find them! |
| ME | Call me when your organization has grown by at least an order of magnitude and your website doesn’t look like it was built by high school students. |
Many years later that organization still has only a few dozen certified therapists in its directory, and yet it remains one of the few and largest directories of its kind. If you live in a big city, there’s a fair to middlin’ chance that you can find one of those therapists. But certification of trigger point therapists is generally an amateurish and fragmented mess, with many businesses and organizations competing to be the standard. (Even this document is part of the mess: a sanity-inducing part of the mess, hopefully, but nevertheless a good example of how everyone and their dog is out there trying to provide “the best” information/training/therapy in this field.)
For inclusion in this section, an organization or business must be defining the field in some way, and they must have a strong online presence.
The relevance of each listing to professional readers and/or patients is marked with [PRO] and [PATIENT]. For instance, although professional associations are rarely of much interest to patients, they may provide directories of professionals to help patients find practitioners.
With apologies to my international readers, this section is mostly American-o-centric. If you are aware of important resources and organizations elsewhere in the world, please let me know.
National Association of Myofascial Trigger Point Therapists ( NAMTPT ) [PRO] [PATIENT] — The only organization dedicated to representing professionals specializing in myofascial pain and trigger point therapy. NAMTPT provides resources for both patients and professionals, such as a trigger point therapist directory ( just over 100 therapists) and a symptom checker.
The International Myopain Society ( IMS ) [PRO] — A nonprofit health professionals organization dedicated to the promotion of information about soft-tissue pain disorders like myofascial pain. IMS publishes the MYOPAIN, a Journal of Myofascial Pain and Fibromyalgia .
American Society of Pain Educators ( ASPE ) [PRO] — A nonprofit organization that trains Certified Pain Educators (CPEs). A CPE educates clinical peers, patients, families, and caregivers on ways to relieve pain by the safest means possible. ASPE training is not focused on muscle pain.
American Academy of Pain Management ( AAPM ) [PRO] [PATIENT] — The largest association of pain professionals in the United States with 6000 members. Similar to the ASPE in that members do not focus on muscle pain in particular: they are included here because they are chronic pain experts in general (although, interestingly, in 2016 they did “spontaneously” form a new “interest group” about myofascial therapy). They provide a directory of members and listings of pain clinics.
Massage Therapy Foundation ( MTF ) [PRO] — A nonprofit organization to advance the profession of massage therapy, founded by the American Massage Therapy Association. The MTF website has a strong focus on research and they publish the International Journal of Therapeutic Massage & Bodywork, which routinely publishes papers about myofascial pain syndrome. Their resources page offers a series of excellent short ebooks by authors I know and vouch for, and I particularly recommend Tracy Walton’s 5 Myths & Truths About Massage Therapy (written for therapists).
The Pressure Positive Company [PRO] [PATIENT] — The best and oldest American manufacturer of good quality massage tools, Pressure Positive has also been a superb corporate citizen, contributing to the advancement of trigger point therapy in many ways, such as collaborating with writers like myself and supporting and promoting scientific research — admirable qualities in a field so often afflicted with pseudoscientific hype. Their website provides many useful resources for both patients and professionals.
Trigger Point Therapy Workshops [PRO] [PATIENT] — A small trigger point workshop provider, for both professionals and patients, notable mainly because the founder is Amber Davies, NCTMB, daughter of Clair Davies and author of The Trigger Point Therapy Workbook — a popular primer on this topic (see my review).
Certification Board for Myofascial Trigger Point Therapists [PRO] [PATIENT] — A small professional organization for trigger point therapists dedicated to “advancing the professional standards of myofascial trigger point therapists through the establishment and maintenance of criteria and procedures for certification.” They offer a modest directory of a few dozen trigger point therapists around the United States.
Neil Asher Continuing Education for Manual Therapists [PRO] — “Neil Asher Technique” is branded approach to trigger point therapy, and the website is mostly built around a directory of NAT certified therapists.
David G. Simons Academy ( DSGA ) [PRO] [PATIENT] — Dr. Simons co-authored the famous big red texts — the seminal text on myofascial pain syndrome — with Dr. Janet Travell. DGSA is named in his honour, and has offered courses in dry needling and manual trigger point therapy worldwide since 1995 (although they seem to be primarily serving Europe). They are hardly the only provider of such workshops, but I single them out because I specifically appreciate their attitude towards certification: they offer to teach skills, not certification levels in a branded treatment “system.” (I don’t necessarily object to branding of training, but I prefer this more academic approach to training.) They maintain a decent bibliography of trigger point research. (See also Seminarios Travell & Simons, offering trigger point courses in Spain led by Orlando Mayoral — there is a regular exchange of experience between DGSA and Orlando Mayoral.)
Myopain Seminars [PRO] [PATIENT] — A post-graduate continuing education company focusing on myofascial trigger points, manual trigger point therapy, dry needling, and trigger point injections. Like DSGA, Myopain Seminars is focused more on teaching skills and knowledge and not a branded certification program, but they do have a directory of graduates of their courses (see their find a clinician feature) and more than a dozen faculty members all “provide high-level diagnostic and management services” for pain patients that may be of interest to many readers of this book. I have a friendly occasional correspondence with founder Dr. Jan Dommerholt, the author of several influential books and papers on this topic; although we don’t necessarily agree on everything — I’m not a fan of dry needling, primarily — I think of him as a mentor and have learned a great deal from him.
Testimonials on health care websites reek of quackery, so publishing them has always made me a bit queasy. But my testimonials are mostly about the quality of the information I’m selling, and I hope that makes all the difference. So here are some highlights from the kind words I’ve received over the years … plus some of the common criticisms I receive, at the end. These are all genuine testimonials, mostly received by email. In many cases I withold or change names and identifying details.
Paul thinks like a scientist, and he’s an excellent writer — a rare and valuable combination. He acknowledges that the trigger point science is “half-baked,” but he’s leaving the door open to debate, unlike some others. And he does this with the humor and aplomb of someone who’s actually read and studied the relevant science and is therefore humbled by it. He also admits that his trigger point manual is his bread and butter, so he’s also transparent about competing interests, which is more than I can say for many clinical researchers in the field of trigger points. Just read his stuff.
John Ware, Physical Therapist
This is, bar none, one of the finest endorsements I’ve ever received. What I particularly love about it is not that it will help sell my book, but something far better: it will help sell it for the right reasons. ~ Paul
Your evidence based approach to pain is to be applauded. You have consolidated and correlated many things that I have previously read as a chaotic patchwork quilt in diverse places and provided valuable additional information and insight that I have not previously found.
Alessandra Campbell
I really appreciate all of the time and effort you have put into your work. I have had arthritis and a hip replacement, with all of the attending issues. My goal has been to seek the proper information to rationally and practically address this. Your work has given me better direction and clarity in understanding some of the body dynamics from an honest perspectice. Many thanks for your work with this.
Phillippa Lutz
First of all thank you for what you do. I stumbled onto your site about six months ago and it has radically changed my perspective on myofascial pain and how I approach and treat patients. In the 16 years I have been a licensed acupuncturist and the 20 before that as a certified massage therapist this is far and away the most useful and eye opening information I have ever come across.
Alishia Livingston
Thank you for your website, it is really a great resource. I have purchased 2 tutorials (trigger points and PF). I also love the concept that you permanently update them and that we have permanent access. I have never seen this concept anywhere else but I find it is really worth the money and better than a book, in the long run.
Bryn Gonzalez
Firstly I would like to thank you for your Trigger Point therapy book, which is very easy to read and follow (and the witty sense of humor doesn’t hurt!).
Yusra Winters
First, thank you for the very informative e-book; I am thoroughly enjoying it — which is strange since it’s a medical text. That attests to your ability to write in a very engaging and easy-to-follow tone.
Safia Salinas
Thank you for delivering information about trigger points and resulting pain in a manner that is understandable to the general public. While I am a Physical Therapist most everything I read or listen to automatically gets translated into a more scientific jargon. This helps me to relay the message to my clients.
Kaydon Joyner, physical therapist
The clarity of your writing is very impressive, and you bring a great attitude to it.
Brittney Taylor
Thank you so much for taking the time to put this book together, and in a way that makes it feel like you wrote it just for me! You have a great writing style.
Hanna Beck
One more noteworthy endorsement, with regards to this whole website and all of my books, submitted by a London physician specializing in chronic pain, medical education, and patient-advocacy (that’s a link to his excellent blog):
I’m writing to congratulate and thank you for your impressive ongoing review of musculoskeletal research. I teach a course, Medicine in Society, at St. Leonards Hospital in Hoxton. I originally stumbled across your website whilst looking for information about pain for my medical students, and have recommended your tutorials to them. Your work deserves special mention for its transparency, evidence base, clear presentation, educational content, regular documented updates, and lack of any commercial promotional material.
Dr. Jonathon Tomlinson, MBBS, DRCOG, MRCGP, MA, The Lawson Practice, London
Oh, I get those too! I do not host public comments on PainScience.com for many reasons, but emailed constructive criticism, factual corrections, requests, and suggestions are all very welcome. I have made many important changes to this tutorial inspired directly by critical, informed reader feedback.
But you can’t make everyone happy! Some people demand their money back (and get it). I have about a 1% refund rate (far better than average in retail/e-commerce). The complaints of my most dissatisfied customers have strong themes:
Thanks to every reader, client, and book customer for your curiosity, your faith, and your feedback and suggestions, and your stories most of all — without you, all of this would be impossible and pointless.
Writers go on and on about how grateful they are for the support they had while writing one measly book, but this website is actually a much bigger project than a book. PainScience.com was originally created in my so-called “spare time” with a lot of assistance from family and friends (see the origin story). Thanks to my wife for countless indulgences large and small; to my parents for (possibly blind) faith in me, and much copyediting; and to friends and technical mentors Mike, Dirk, Aaron, and Erin for endless useful chats, repeatedly saving my ass, plus actually building many of the nifty features of this website.
Special thanks to some professionals and experts who have been particularly inspiring and/or directly supportive: Dr. Rob Tarzwell, Dr. Steven Novella, Dr. David Gorski, Sam Homola, DC, Dr. Mark Crislip, Scott Gavura, Dr. Harriet Hall, Dr. Stephen Barrett, Dr. Greg Lehman, Dr. Jason Silvernail, Todd Hargrove, Nick Ng, Alice Sanvito, Dr. Chris Moyer, Lars Avemarie, PT, Dr. Brian James, Bodhi Haraldsson, Diane Jacobs, Adam Meakins, Sol Orwell, Laura Allen, James Fell, Dr. Ravensara Travillian, Dr. Neil O’Connell, Dr. Tony Ingram, Dr. Jim Eubanks, Kira Stoops, Dr. Bronnie Thompson, Dr. James Coyne, Alex Hutchinson, Dr. David Colquhoun, Bas Asselbergs … and almost certainly a dozen more I am embarrassed to have neglected.
I work “alone,” but not really, thanks to all these people.
I have some relationship with everyone named above, but there are also many experts who have influenced me that I am not privileged to know personally. Some of the most notable are: Drs. Lorimer Moseley, David Butler, Gordon Waddell, Robert Sapolsky, Brad Schoenfeld, Edzard Ernst, Jan Dommerholt, Simon Singh, Ben Goldacre, Atul Gawande, and Nikolai Boguduk.
Thank you finally to Dr. Tim Taylor, MD, who provided a great deal of the raw material that went into the original version of the book’s vital sections medical factors that perpetuate pain.
Regular updates are a key feature of PainScience.com tutorials. As new science and information becomes available, I upgrade them, and the most recent version is always automatically available to customers. Unlike regular books, and even e-books (which can be obsolete by the time they are published, and can go years between editions) this document is updated at least once every three months and often much more. I also log updates, making it easy for readers to see what’s changed. This tutorial has gotten 197 major and minor updates since I started logging carefully in late 2009 (plus countless minor tweaks and touch-ups).
2021 — Polishing: Long overdue proofreading of the entire book, correcting several dozen typos that have snuck into it over the years. This is by far the longest of my books, and so it had by far the most typos, and no doubt there are still a few — but it’s greatly improved. Also for this project, I updated all references made to my work as a massage therapist, a great many of which still read like I have appointments schedule next week, when in fact I haven’t seen massage therapy client in over a decade now.
2021 — Added anecdote: Added a solid anecdote from a physician reader about “appendicitis” cases treated with lidocaine injections in the abdominal muscles. Also added some extra medical information about pain in this area. [Updated section: Trigger points may explain many severe and strange aches and pains.]